In haemostasis, even more than any other disciplines, quality in test reporting is determined by a very significant step i.e pre-analytical
Pre-analytical errors may occur throughout the testing process and arise from unsuitable, inappropriate or wrongly handled procedures.
The accurate standardization of the pre-analytical phase is of pivotal importance for achieving reliable results of coagulation tests and should reduce the side effects of the influence factors. Let’s therefore summarize the recommendations regarding the importance of pre-analytical factors for coagulation testing and hoping that it increases the awareness about the importance of pre-analytical factors in coagulation testing.
Sample collection/ Haematocrit adjustments
The order of drawing blood during phlebotomy should be
- Blood culture/
- Sterile tubes,
- Coagulation tubes,
- plain tubes/gel tubes, then
- Tubes containing additives.
Draw a discard tube when citrated plasma is obtained using butterfly systems or other IV catheter devices.
- Ensure correct filling of tubes (>90% filling).
- Following collection, blood should be adequately and promptly mixed by 3-6 complete end-over-end Inversions
- If the hematocrit is between 55% and 65%, it is acceptable to remove 0.1 mL of the citrate anticoagulant from the tube and not perform the calculations.
- For those patients with hematocrit >65%, use the following formula to determine the correct anticoagulant volume: C = (1.85 × 10–3)(100 – HCT)(V Blood)
Abbreviations: C= volume of citrate remaining in the tube, HCT = patient’s hematocrit, and V = the volume of blood to be added. (If a 5-mL tube is used, V= 4.5 mL)
Sample processing
- Immediately upon collection the phlebotomist shall adequately and promptly mix the blood tube by 3 to 6 complete end-over-end inversions of the tubes in order to ensure complete distribution of anticoagulant.
- Avoid vigorous shaking, vortexing or agitation of blood samples.
- Adjust the citrate volume in case of high haematocrit (remove part of the citrate solution from the sampling tube prior to drawing blood).
- Check tubes for presence of clots, precipitates or haemolysis.
Sample Storage
- Sample rejection policy should be established and followed strictly.
- Centrifuge the primary tube for coagulation testing at 1500g, 20 min (3500 RPM assuming the radius of rotor to be 10cm) for 20 minutes. For conversion of Relative Centrifugal Force (RCF) or g force to RPM click on the below link for easy conversion in values:
- Samples for aPTT should be performed using fresh plasma <4 h (<1 h in patients treated with unfractionated heparin).
- Do not perform PT, aPTT and factor VIII tests from frozen samples. Plasma samples frozen at minus 20 °C remain stable for 2 weeks. Plasma frozen at minus 80 °C remains stable for 6 – 18 months dependent on the parameter.
- Avoid freeze-thaw cycles more than once. Use aliquots instead
Time from sampling to analysis depends on analyte:
- Samples for PT/INR have longer stability (24 h) at room temperature.
- Samples for aPTT should be performed using fresh plasma <4 h (<1 h in patients treated with unfractionated heparin).
- For platelet function assays, samples should rest at room temperature for at least 15 min before analysis. Testing should be completed <3–4 h of collection.
- For factors V and VIII analyses should be performed <3 h.
- Fibrinogen, protein C and antithrombin activity appear to remain relatively constant when stored at room temperature for up to 7 days.
- Protein S activity is unstable, with a statistically significant loss of activity at 8 h.
- VWF appears to be stable at room temperature for 48 h.
Transportation of samples
- Before transport, test samples regarding identification, safety conditions and stability.
- Transport samples at ambient temperature (15–25 °C) in as short a time as possible.
- Draw samples directly in a laboratory.
- Immediately after drawing, whole blood should remain capped for transport.
- Temperature control is recommended in rooms where samples are kept for analysis.
- Transfer samples vertically.
- Do not use pneumatic tube systems (PTS) for transport of samples used for platelet function analysis.
Specimen rejection
- All samples deemed unacceptable due to pre-analytic handling and unfulfilled transport requirements should be rejected.
- Inappropriate collection tubes and additives.
- Outdated tubes.
- Error in patient identification or lack of identification.
- Insufficient volume (depending on the assay). An alternative may be to adapt the result depending on the additional dilutional (e.g. for factor assays, fibrinogen).
- Haemolysed specimens (depending on the assay).
- Identification of a clot.
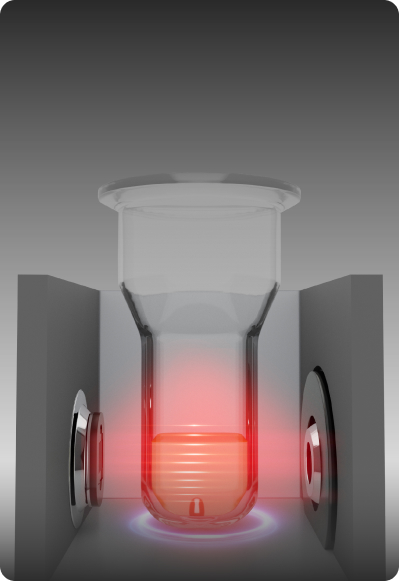
Centrifugation
- Use a temperature-controlled centrifuge for processing routine coagulation assays.
- Validate the centrifuge before use, every 6 months or after modifications, in order to assure that platelet-poor plasma (PPP) is achieved.
- Check the absence of vibration (during acceleration/deceleration processes) due to lack of centrifuge maintenance.
- Centrifuge the primary tube for coagulation testing at 1500g for 20 min
- In case of emergency, for PT, APTT and fibrinogen performed on fresh plasma, higher centrifugation force 2500g for 10-12 min can be used.
- The preparation of PPP requires a double centrifugation to obtain a residual platelet count lower than 10×109/L. Following initial centrifugation, transfer carefully the plasma to a non-activating plastic centrifuge tube using an automatic pipette, and then centrifuged again for about 15 min.
- The preparation of platelet-rich plasma (PRP) for platelet function analysis requires a centrifugation performed at 200–250 g for 10 min without application of a rotor brake.
Conclusion
Continuous monitoring and management of pre-analytical errors is crucial in order to improve the quality of the pre-analytical phase, which is essential for patient care. Standardization efforts are essential to control and prevent errors and to ensure the quality of exploration in haemostasis.
The effects of pre-analytical variables on the reliability and consistency of screening tests is often forgotten due to a lack of understanding and awareness. This can be improved by educating healthcare professionals who are involved in drawing blood for testing.
Stay tuned for more….
Review/comment or simply ask a question on any of the topics to Mr.Shariff.